Are you on Medicare? Do you have Part B?
It may seem like a silly time to ask that question. The annual enrollment period just ended December 7th. But getting insured doesn’t always require waiting for an annual enrollment period. In today’s blog, I’ll summarize the exceptions…
#1 – If you are under 65 and healthy, Medicare is probably not what you want. What you want is Obamacare. Obamacare goes by a few other names – ACA, Marketplace, FFM. Don’t be confused. I’m here to make it all easier to understand. There is an open enrollment period for the Federally Facilitated Marketplace (FFM), (or your state marketplace, if you are in a state with a state FFM equivalent). For most people, it’s understood as Obamacare. But what’s in a name? Bottom line: your enrollment period ends January 15th. Call me. I’ll show you your options.
#2 – Some insurance products don’t have enrollment periods. For instance, odds are you can sign up for an indemnity plan any time of the year. You can also add on or remove dental, health and vision, or cancer, heart attack and stroke policies to your existing insurance. Obamacare and Medicare plans don’t normally cover these. You can also initiate a Health Matching Account at any time up to age 64 without respect to enrollment periods.
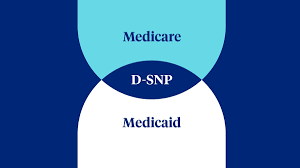
#3 – You may qualify for Medicaid. And if you qualify for both Medicaid and Medicare, you may be eligible for a Dual Special Needs Plan (D-SNP) with a Dual Special Enrollment Period (D-SEP). I have a heart for people in need. And the good news is that those who qualify, can enroll or change plans once every three months – except in the fall. But that’s when the Annual Enrollment Period (AEP) happens (Oct. 15th-Dec 7th), so even in the fourth quarter you can get enrolled or change plans if you are a Medicaid recipient who qualifies for Medicare.
#4 – Whether it’s Obamacare, or Medicare, if you move in or out of a service area, you’ll probably qualify for a special enrollment period (SEP). In fact, if you don’t change plans, carriers will boot you off your plan after you’ve been out of the area for six months. Don’t let this catch you off guard. Go ahead and change plans before or after your move. Ideally, you’ll remember to set an effective date for a health plan change a few months in advance as you are packing. I love getting calls from people moving to Tallahassee. I’m happy to be their tour guide.
#5 – You also qualify for a Special Enrollment Period if your plan gets terminated. Moving can do that. So can non-payment. Don’t let your policy lapse! Other reasons might involve fraud or duplicate coverage. Maybe your plan’s carrier went out of business. Or on a more positive note – if you were on a special needs plan for a chronic condition that you no longer qualify for, or because your icnome improved and you no longer qualify for a Dual Special Needs Plan. Whatever the reason, the good news is you may not have to wait until next year to get insurance.

#6 – Thinking even more positively, there’s also the possibility that a plan earned five stars. A plan earns five stars when it doesn’t get bad reports from enrollees. Companies that get compliments instead of complaints through the Center for Medicare and Medicaid toll free number get rated accordingly. When a company earns five stars, everyone in the network area has the option to immediately switch to that plan, or do so any time before the next annual enrollment period. Cool? Believe it or not, there is actually some incentive for these networks to meet or exceed your expectations. I should also disclose that part of that formula is agents like me. If I tell you about a plan, I want to make sure you get out of it what you are hoping for. Good communication is critical. Complaints stem from poor communication. Never rush when enrolling in health care. Learning about it can be a tedious process. There are too many choices. I’ve learned that good communication and consumer education is an art. It may be faster to just say, “trust me.” I can get people in and out of the door quickly if I have to. But medical costs and processes have harsh realities. I’ve done my job well if I’ve prepared you to know what to expect. Take time for quality decision making. Five stars.
#7 – Dramatic changes in your health or income may also qualify you to change plans outside of the annual enrollment period. This can be an improvment from a chronic or qualifying condition that triggers the loss of a plan as noted above (#5), or it can be a loss of health that qualifies you for a chronic special needs plan (C-SNP). There is also going into or coming out of institutions such as nursing facilities. This will trigger a thirty day period to change a plan under an I-SNP (SEPI). Don’t worry about the jargon and the acronyms. Just call me and I’ll give you more specifics.
#8 – Federally Declared Emergencies and Disaster Areas can trigger special enrollment periods. In Florida, we had Hurricane Idalia. This SEP declaration is effective: 08/27/2023 – 01/31/2024. All counties in the state qualify.
#9 – When we are talking about Medicare, there is always a bit of confusion about the difference between an Intital Eligibility Period (IEP) and an Intial Coverage Enrollment Period (ICEP). This relates to when a person actually enrolls in or qualifies for and takes advantage of Medicare for the first time as opposed to when they become eligible. A person becomes eligible three months before their 65th birthday to sign up for Medicare. This is the Initial Eligibility Period (IEP). It lasts until the end of the third month after their birthday and it comes in two possible parts – Part A and Part B. Part A is automatic and free when you request it from Social Security at https://ssa.gov.
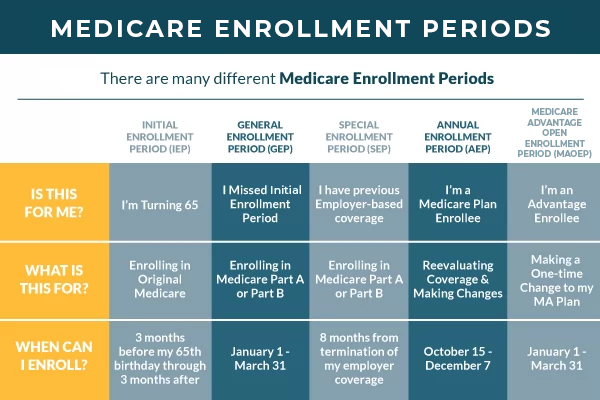
Part B is optional and some people delay paying it because the premium is pretty significant. You may be penalized if you don’t pay it. You may have an equivalent from your employer’s group health plan. If you do, you won’t be penalized. The catch is that you still have to pay for Part B if you want a Medicare Advantage plan. And there are certain advantages to Advantage plans, but today we’re just talking about special enrollment periods, and the ICEP isn’t exactly a Special Enrollment Period (SEP). It’s standard. But both the IEP and the ICEP periods give certain qualifying individuals time outside of Annual Enrollment Period Oct. 15th – Dec. 7th, to enroll in or change Medicare plans. And that’s my summary of special enrollment periods.
#10 – When you do things matters. You can call me any time and ask for help. You can get all this same information at Medicare.gov and/or at CMS.gov. HealthCare.gov focuses mainly on Obamacare and the Marketplace or FFM. I am here to guide you through it all. Two other periods deserve special mention. For Medicare, there is an Open Enrollment Period (OEP) from Jan. 1st – March 31st. The Medicare Advantage Open Enrollment Period is for those on Medicare Advantage Plans. Whereas during Annual Enrollment period those qualified can make as many changes as they want until the period ends, Medicare recipients can make only one change during the Medicare Advantage OEP period. They can go back to traditional Medicare if they want. Or they can switch Medicare Advantage plans. If they go back to traditional Medicare, they can add a stand alone drug plan. The purpose of this period is to help people make adjustments when they’ve chosen plans they realize don’t really meet their needs.
The second special period is for Obamacare. This is the regular Open Enrollment Period for the Marketplace that begins November 1st and lasts until January 15th. We are now in that period. In my last blog, I described the various health care buckets. It is not always in a person’s best interset to be on a Marketplace plan. Private plans that don’t qualify for the Marketplace may be both less expensive and even cover more, depending on the plan. I already covered this a few blogs ago so I won’t repeat that here. Today, I just wanted to be clear about when to take action. In December and early January, I’ll be focusing my attention on the young and the relatively healthy since its open season. I do have contracts with a number of Maretplace carriers and plans, not all. But I also know most people want to save money. Call me and I’ll show you your options.